Infertility and the Medical Aspects of Third Party Reproduction
By Carrie Bedient, MD, FACOG
The Fertility Center of Las Vegas
Overview
Starting a family is a central focus in many cultures, and an inability to do so may cause personal distress and relationship disruption. Historical treatments in managing fertility focused on perceived character weakness or faults of the woman and appeasing an angered deity thought to be withholding the ability to have children. Thankfully, over several hundred years science evolved and through further investigation determined that conception relied upon multiple factors working in concert to achieve a healthy child. The most significant result of these investigations culminated in 1978 with the birth of the first baby via in vitro fertilization. Initial success rates with fertility treatments were quite low. However, subsequent advances have greatly increased success rates. Current research focuses on improving pregnancy rates, safeguarding the health of both intended parents and the fetus throughout the process, and developing diagnostic techniques to prevent genetic diseases in the child.
Infertility
The American Society of Reproductive Medicine defines infertility as “the failure to achieve a pregnancy after 12 months or more of appropriate, timed intercourse or therapeutic donor insemination”. Patients over the age of 35 should undergo evaluation after six months of attempting conception and patients over 40 years should have an immediate evaluation. 15% of couples may experience difficulty conceiving. These difficulties may be due to male factor (few or no sperm, no moving sperm), female factor (poor quality or absence of eggs, blocked tubes, abnormal uterus, or hormonal factors), or a combination of both.
Key components required for fertility include eggs (oocytes), sperm and a uterus. Fertility without medical assistance also requires open fallopian tubes to allow fertilization and transport of the egg and sperm. Societal changes such as older age at the time of marriage, delayed childbearing for personal or professional reasons, and the publicity accorded to celebrities who successfully become pregnant later in life (often using assisted reproduction techniques) have led to greater occurrence of patients waiting to conceive. Unfortunately, despite these societal changes, physiology remains the same and can lead to difficulties conceiving when patients wait too long to attempt pregnancy. Additionally, same-sex couples and patients who have undergone significant medical treatments (i.e. hysterectomy or chemotherapy) may need assisted reproduction techniques to help grow their families.
Diagnostic testing to help determine the cause of infertility includes:
Male factor: All males should have a semen analysis to determine the number of sperm and their ability to move. Hormonal assessment or evaluation by a urologist may also be necessary.
Ovarian reserve: These tests help determine the quantity and quality of eggs in the ovary. Lab tests are an FSH and estradiol level drawn on the third day of the menstrual cycle, and an AMH (anti-mullerian hormone) level that can be drawn at any time. An antral follicle count is obtained by vaginal ultrasound in the early part of the menstrual cycle.
Tubal testing: The fallopian tubes can be assessed by an x-ray with dye called a hysterosalpingogram (HSG). This determines if the tubes are open and of normal size. The tubes can also be assessed during laparoscopic surgery.
Uterine testing: The uterus should be evaluated for shape and capacity to carry a potential pregnancy, which can be assessed by an ultrasound. In specific cases an ultrasound combined with saline in the uterus can also be very helpful.
Your fertility center will also determine what additional lab tests are needed to assess hormonal status, history of infections and immunity, or other tests specific to you and your partner.
Approximately 1/3 of patients have male factor infertility, 1/3 have female factor infertility and 1/3 have a combination. The cause of infertility is not always found by testing, however, treatment is frequently successful even when no cause is identified.
Common diagnoses
Ovulatory dysfunction: This refers to any disorder that prevents release of an egg every month (for example: polycystic ovarian syndrome, premature ovarian failure).
Male factor: This includes a lower number of sperm (oligospermia), absent sperm (azoospermia), or sperm that are unable to move properly (asthenospermia). These changes in sperm can be due to a blockage in the male reproductive tract, hormonal imbalances or genetic conditions.
Uterine pathology: This includes fibroids or polyps that distort the inside of the uterus. It also includes abnormalities in the shape of the uterus, such as a septum, bicornuate or arcuate uterus.
Endometriosis: This is tissue from the lining of the uterus that implants on the ovaries, outside of the uterus and in the pelvic cavity, causing scar tissue that interferes with egg release and transport. It is also associated with ovarian cysts called endometriomas that may impact ovarian reserve.
Tubal disease: Blockage or damage to the fallopian tubes resulting from infection, scar tissue or prior surgery may prevent egg and sperm transport.
Unexplained: Up to 30% of couples with infertility may not have any abnormalities on diagnostic testing. Despite not knowing the specific origin of infertility, these couples still do well with infertility treatments.
FAQs
What testing do I need to do?
- Ovarian reserve testing: Lab tests of AMH, day 3 FSH and estradiol, ultrasound for antral follicle count
- Tubal status: x-ray with dye (hysterosalpingogram)
- Semen analysis
- Uterus: ultrasound or sonohysterogram
- Preconception labs: It is a good idea to check general health status before attempting pregnancy; this can include immunity to disease, infectious testing, blood type, etc
How long does diagnostic testing take?
Diagnostic testing usually takes a few weeks to complete, depending on where you are in the menstrual cycle.
What type of treatment should I ask for?
You want the best treatment for your specific problem and for you as a person, and that will depend on results of all testing and discussions with your doctor.
How do I know if a treatment center is good?
The most important factor is comfort with your doctor and the treatment team, as this can be a stressful process. Look for a board certified reproductive endocrinology and infertility physician and meet with them to discuss your case. Fertility clinic success rates can be found at sart.org or cdc.gov/art.
When should I get tested?
If you have no known risk factors for fertility problems – after 12 months of attempting conception. If you are over 35 years old, see a fertility clinic after 6 months of trying. If over 40 years old, please see a clinic as soon as you decide to conceive.
Treatment Options
Medications: Frequently used oral medications include clomiphene citrate and letrozole. These pills are taken for 5 days during the cycle, then an ultrasound is performed to ensure appropriate growth of follicles. Additional medications include injections to help stimulate the eggs to grow in the ovaries, and medications to induce ovulation. A full evaluation is needed before prescribing these medications.
Insemination: Insemination is placing sperm directly in the uterus at the time of ovulation to improve chances of conception. The sperm may come from the male partner, from a sperm donor, or some from both. The sperm sample is “washed,” meaning the highest quality sperm is separated and concentrated before insertion. The IUI process is easy, quick, and usually painless. Intrauterine Insemination can be performed during a natural ovulation cycle, but may work best if a regimen of medications is employed first to promote the development of more ovarian follicles. After the administration of the ovulation induction medication, the follicular development is monitored by pelvic ultrasound. The final sperm sample will be placed inside the endometrial cavity using a catheter specially designed for IUI.
In Vitro Fertilization (IVF): In most cases, In Vitro Fertilization begins with ovarian stimulation. During this process, medication is used so that the patient’s ovaries are stimulated causing follicles to develop. The eggs in the follicles are then matured, removed, and fertilized with sperm in the laboratory. Once fertilized, the embryos are then grown in carefully controlled laboratory conditions until they are ready to be implanted into the uterus. While in the laboratory, the embryos are evaluated, and the most viable embryos are selected for transfer to the uterus. Any remaining viable embryos may be frozen for later use.
Frozen Embryo Transfer is most often done with excess embryos remaining after the transfer of fresh embryos. If the fresh transfer fails or if it succeeded and the patient wishes to return to try to have more children, then the frozen embryos may be thawed and transferred. In many cases, all of a patient’s embryos may be frozen. It has been shown that many patients can have improved success rates with transfer of frozen-thawed embryos than fresh embryos. When the patient is ready, their uterus will be prepared with hormones, including estrogen and progesterone. At the proper time, the embryos will be thawed, examined, and transferred.
Intracytoplasmic Sperm Injection: This occurs during IVF when the sperm is injected directly into the egg to help facilitate fertilization, and is particularly useful when the number or motility of sperm is decreased.
Sperm extraction techniques: In some cases of obstructive azoospermia (i.e. with prior vasectomy or congenital bilateral absence of the vas deferens), sperm may be extracted from the testicles or epididymis for use in IVF with ICSI. This is typically done by a urologist specializing in male infertility working with a reproductive endocrinologist and embryologist.
Third party reproduction – Egg Donors, Sperm Donors and Gestational Carriers
In Vitro Fertilization is a versatile procedure. The eggs used in the procedure can come from the intended parent, or they can come from a third party egg donor. Likewise, the sperm may also come from the intended parent, or from a third party, sperm donor. Furthermore, the fertilized embryos may be transferred to the uterus of the intended parent or to the uterus of a carefully selected gestational carrier who carries the pregnancy for the parent(s), if necessary. IVF can be attempted using either fresh or frozen embryos. IVF has been successful in providing children to women with no male partner, to men with no female partner, and to same-sex couples. IVF also allows intended parents the option of pre-implantation genetic diagnosis and screening of embryos to reduce the risk of having children with genetic diseases.
Egg Donors
Oocyte donors are women who choose to provide their eggs so that other women can have children. In some cases, the egg donor is a family member of the patient, but more often the donor is anonymous. All egg donors are screened for infectious diseases to reduce the risk that their eggs could transmit a disease to the patient. The Fertility Center of Las Vegas maintains a ready set of anonymous donors so that there is usually no waiting for a patient that needs a donor.
In a donor egg cycle, the donor is stimulated so that they will produce many follicles and many eggs. The eggs are collected and fertilized, and the best embryos are transferred to the patient. The two cycles are synchronized so that the embryos are ready for transfer when the patient’s uterus is ready to receive them. Any viable remaining embryos may be frozen for future use. Egg donor cycles produce excellent success rates.
Sperm Donors
For a single female patient, lesbian couples or heterosexual couples with male-factor infertility, a sperm donor can be selected from a sperm bank or a known donor (screening required). We will assist you in the process of obtaining donor sperm and can help arrange for shipment and storage of the specimen prior to treatment. Once the donor sperm is received, it will then be used in an insemination (IUI) cycle or with an In Vitro Fertilization (IVF) cycle.
Gestational Carriers
A Gestational Carrier (GC) or Surrogate is a woman who agrees to carry a baby through a pregnancy for an individual or couple. The GC only provides a host uterus for the baby but does not contribute genetic material. The embryo is created using an egg from a female intended parent or an egg donor. The egg is fertilized by using sperm provided by a male partner or a sperm donor. IVF with Donor Egg & Gestational Carrier/Surrogate can be performed for a variety of individuals including: single females, lesbian couples, gay couples and heterosexual couples.
Female Patients
Sometimes a woman cannot physically carry a pregnancy due to uterine cancer, a uterus damaged by infection, congenital uterine abnormalities or another health issue that prevents the mother from carrying a baby. In these cases, she may choose to have another woman (gestational carrier) carry the pregnancy and deliver the baby for her. The gestational carrier must have a healthy uterus. A gestational carrier may be a family member, a friend or a compensated or non-compensated volunteer. Both the parents and the gestational carrier must be screened for infectious diseases, and the carrier is also psychologically screened.
The intended mother and the gestational carrier undergo a synchronized cycle, exactly like an egg donor IVF cycle, so that the mother’s embryos are ready to transfer when the carrier’s uterus is ready to receive them.
Male Patients
A gestational carrier is an excellent option for single men and gay families looking to create their families. At The Fertility Center of Las Vegas, we can assist you with every aspect of the process. From finding your surrogate, finding the appropriate legal guidance for your home state or your home country, use of donor egg and/or donor sperm, patient screenings through to conception, our team of surrogacy and legal experts will walk you through each step of the process so that you can focus on your new family. Your gestational carrier may be a family member, a friend or a compensated or non-compensated volunteer. The parent(s) and the gestational carrier must be screened for infectious diseases, and the carrier is also psychologically screened.
Pre-implantation Genetic Diagnosis/Pre-implantation Genetic Screening
Pre-implantation Genetic Diagnosis (PGD) and Pre-implantation Genetic Screening (PGS) are genetic tests combined with the IVF process to diagnose an embryo before embryo transfer for an abnormal number of chromosomes or known genetic mutations. Embryos that are free of genetic abnormalities can then be selected for transfer to the uterus.
The most common abnormality in embryos is called aneuploidy. Aneuploidy is when there are too many or too few chromosomes and can lead to:
- Failed pregnancy
- Miscarriage
- Termination of pregnancy
An estimated 70% of early miscarriage is associated with a chromosomal abnormality in the fetus. Some studies suggest genetic testing before embryo transfer helps to achieve higher implantation rates, fewer pregnancy losses and lowers the risk of having to consider pregnancy termination. Patients who may benefit from PGS include:
- Women 35 years of age or older using their own eggs
- Women with repeated miscarriages
- Patients with multiple failed IVF cycles
- Patients who have had a previous pregnancy involving a chromosomal abnormality.
The Fertility Center of Las Vegas uses advanced PGS, which involves the removal of a few cells from a blastocyst embryo (day 5 or 6). The biopsied cells are then evaluated for all 23 pairs of chromosomes. Normal embryo(s) are then selected for transfer to the patient. This procedure of biopsying the embryo at a more advanced cell stage (blastocyst) significantly increases the accuracy of the testing and minimizes potential damage that the biopsy can cause on the embryo. By waiting until the embryo reached the blastocyst stage, the embryologist will only need to remove a small portion of the embryo mass which is removed from the placental cells rather than fetal cells.
Medical or Elective Gender Selection
In addition to selecting chromosomal normal embryos, PGD/PGS can also identify the gender of the embryo. Gender selection can be elective or for medical reasons. Elective gender selection is made when the parents have a preference in the child’s sex and for family balancing. Medical gender selection can be beneficial for patients who have a family history of a specific sex linked disease. For example, muscular dystrophy and hemophilia are inherited by the mother but only affect male offspring. Certain other conditions impact one sex more than the other (Fragile X syndrome, autism, etc.)
Egg Cryopreservation
Although ovaries can decline at any time, even in our 20s, the average woman begins to experience decline starting around age 33 to 35. By their early 40s, most women’s ovaries have declined greatly. Egg freezing is an important option for these women to preserve their fertility. Egg freezing involves stimulating the ovaries to produce follicles and eggs, removing these eggs and freezing them. Multiple egg retrievals may be employed to get a large set of frozen eggs, which increases the chance of later success. Frozen eggs may be safely stored for many years without any known harm. The eggs may be thawed, fertilized with sperm from a male partner or donor sperm and transferred to the uterus when the woman is ready. Couples who wish to preserve fertility, but are not ready to have children, may choose to freeze eggs or embryos. Women who are preparing to undergo cancer treatments that might harm their ovaries also often utilize egg or embryo freezing.
Success Rates
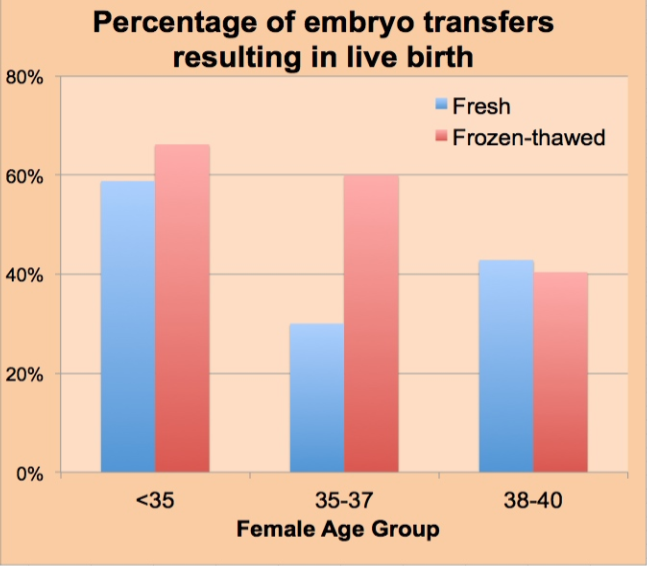
Success rates depend heavily on the age of the woman providing the eggs. The rates of live birth for women using their own eggs at The Fertility Center of Las Vegas in 2013 (the latest results available as this is written) are shown in the graph below. For women using eggs from an egg donor, the birth rates per embryo transfer that year were 65% and 69%, respectively.
Dr. Carrie Bedient, Contributing Medical Specialist
Dr. Carrie Bedient is a Reproductive Endocrinology and Fertility specialist at the Fertility Center of Las Vegas. She graduated from the University of Arizona College of Medicine, and went on to train in Obstetrics and Gynecology at the Cleveland Clinic Foundation and Metrohealth Medical Center in association with Case Western Reserve University School of Medicine. Dr. Bedient completed fellowship training at Emory University before returning to the west to join the Fertility Center of Las Vegas. Her research includes immune cell function in endometriosis, as well as fertility testing in pediatric patients who have received cancer treatment. Dr. Bedient is a member of the Gold Humanism Honor Society and has received awards for excellence in research and laparoscopy. She is a member of ASRM, ACOG, PCRS, and SART.
Fertility Center of Las Vegas
The Fertility Center of Las Vegas, Henderson and Los Angeles (http://www.fertilitycenterlv.com) was founded in 1988 by Dr. Bruce Shapiro, with Dr. Said Daneshmand joining in 1999. They have most recently welcomed Dr. Carrie Bedient to their practice. Together they have helped create thousands of families by providing the most advanced fertility treatments available today. They are a full service clinic offering traditional and third party solutions with offices in Nevada and California. For information call +1-702-254-1777 or visit their website at fertilitycenterlv.com/contact-us/.
